Endotracheal intubation
1.8.1. Indications for intubation
If the infant’s heart rate does not rise above 60 beats per minute with chest compressions and effective positive pressure ventilation in 100% oxygen, then advanced resuscitation interventions (including drug administration) are now indicated.
The administration of drugs requires that the infant has intravenous access or an endotracheal tube in-situ. The indications for endotracheal intubation and umbilical vessel catheterisation are discussed below.
The skills of intubation and umbilical vessel catheterisation are considered to be advanced resuscitation interventions. The opportunity to practice and apply these skills is offered to participants undertaking the Advanced Resuscitation Program.
Endotracheal Intubation
There is no “set” or correct time to decide to intubate a newborn infant during a resuscitation, although there are several circumstances in which intubation is indicated if a person with the professional expertise to perform this procedure is available. These are:
- Mask ventilation (with a T- piece device, bag or laryngeal mask) is difficult or does not result in the infant’s heart rate increasing to above 100 bpm and the newborn has not made adequate breathing efforts
- The infant is born without a detectable heart rate
Intubation under specific circumstances
- The infant born through meconium stained amniotic fluid who is not vigorous at birth may be intubated and receive brief tracheal suctioning if a person with the expertise to perform this procedure is available.
- The preterm infant born in a tertiary centre may be given CPAP from birth via a mask and/or nasal prongs or intubated soon after birth so that surfactant can be administered
- See Resuscitation in Special Circumstances for more information
Equipment for endotracheal intubation
- A full set of intubation equipment should be available in all areas of hospitals where babies are born
- At all high risk births, this equipment should be set up ready for use and a person with the expertise to intubate should be present at the birth
- Click here for a list of the recommended equipment for endotracheal intubation
Endotracheal size and length
|
Weight in grams
|
Gestation in weeks
|
Tube size: Internal diameter in mm
|
Depth of insertion from upper lip in cm
|
| < 1000 | < 28 | 2.5 | 6.5 – 7 |
| 1000 – 2000 | 28 – 34 | 3.0 | 7 – 8 |
| 2000 – 3000 | 34 – 38 | 3.0 or 3.5 | 8 -9 |
| > 3000 | > 38 | 3.5 or 4.0 | < 9 |
The endotracheal tube diameter can also be calculated using the infant’s gestational age in weeks divided by 10.
Click here to access the Neonatal Worksheet, which will calculate the correct size endotracheal tube and depth of insertion for a given gestational age and birth weight.
Estimating the depth of insertion of the endotracheal tube
The “rule of 6” can be used as an estimate as to where the endotracheal tube should be tied.
| “Rule of 6” | Length at which the tube should be tied at the lips or nares in cm |
| Oral intubation | Infant’s weight in kg plus 6 cm = length at the lip |
| Nasal intubation | Infant’s (weight in kg x 1.5) plus 6 cm = length at the nares |
Oral versus nasal intubation
- Oral intubation is recommended in an emergency situation as it is easier and quicker than nasal intubation in most instances.
- Nasal intubation should only be attempted by personnel experienced in and proficient at nasal intubation.
Verification of endotracheal tube position
- ANZCOR state: An end tidal CO2 detector attached to the outside end of the endotracheal tube is recommended for verification of correct tube placement in neonates who have spontaneous circulation. (Guideline 13.5, 2016)
- Positive detection of exhaled CO2 via a colorimetric carbon dioxide detector (e.g. Pedi-Cap™ CO2 detector or similar) attached between the end of the endotracheal tube and the manual ventilation device confirms tracheal intubation.
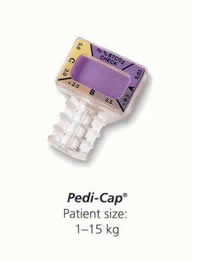
Nellcor/Tyco Healthcare
Pedi-Cap™ CO2 detector (1kg – 15kg Pediatric)
You may wish to view the Pedi-Cap CO2 detector presentation on the NeoResus web site.
Other clinical signs that indicate successful tracheal intubation
- The infant’s heart rate rises quickly to above 100 bpm with positive pressure ventilation via the endotracheal tube.
- The endotracheal tube is visualized passing through the vocal cords.
- Breath sounds are heard in both axillae with a stethoscope
- This can be misleading in a preterm infant as sound is easily transmitted. Sound heard over the anterior portion of the chest can be coming from the stomach or oesophagus
- Breath sounds should be absent or decreased over the stomach
- In certain circumstances, such as a pneumothorax or congenital diaphragmatic hernia, there may be asymmetrical breath sounds
- Vapour (mist) is seen on the inside of the endotracheal tube during exhalation
- N.B. The presence of misting inside the endotracheal tube has not been systematically evaluated in neonates (ILCOR, 2006)
- Symmetrical chest movement is seen with each positive pressure inflation
- Lack of symmetrical chest movement may indicate that the tip of the endotracheal tube has been inserted too far (usually in to the right main bronchus) and needs to be withdrawn to the correct distance
- The newborn’s colour will improve
- Note that in certain conditions, such as the infant with congenital heart disease associated with decreased pulmonary blood flow, or PPHN pattern, the infant’s colour may not improve, despite the endotracheal tube being correctly positioned in the trachea
The “gold standard” of verifying correct endotracheal tube placement
- A chest X-ray is the gold standard of confirming that the endotracheal tube is in the trachea and inserted to the correct depth.
- The Pedi-Cap™ CO2 detector will confirm endotracheal tube placement in the trachea (as opposed to the oesophagus) but will not confirm the correct position of the tube, which should be midway between the vocal cords and the carina (thoracic vertebrae T2- T3). This can only be confirmed with a chest X-ray.
- A chest X-ray should be performed once the infant has been admitted to the Special or Intensive Care Nursery (See Investigations and imaging in Learning Module 4 for more information).
|
Clinical Practice Guidelines for Intubation
Victoria: Better Safe Care: Neonatal eHandbook. Intubation (Updated July 2019)
| Previous | Next- Supraglottic airway |
